Sleep apnoea and digital connected health
Patient engagement using new technology to improve adherence to positive airway pressure therapy.
Malhotra A, et al. CHEST 2017.
The study: An observational study of over 128,000 people with sleep apnoea whose devices allow for remote monitoring of therapy by their clinician or by the patients themselves via myAir, ResMed’s cognitive behaviour-based patient engagement app for web and iPhone®.
Findings: In a research study presented at the 2016 CHEST Congress of the American College of Chest Physicians, ResMed shared evidence that people who use online self-monitoring tools when treating their sleep apnoea with positive airway pressure (PAP) are significantly more likely to stick with their therapy.
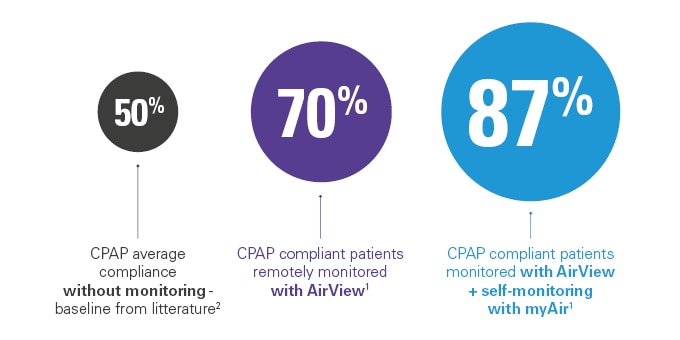
- More than 87% of patients who used ResMed myAir and were monitored through ResMed AirView stayed with their therapy over 90 days.1
- Patients who did not use myAir but were monitored through AirView still improved their compliance levels: 70% instead of an estimated 50% CPAP average compliance without monitoring – baseline from literature.1,2
“This new study shows that online self-monitoring tools engage patients and significantly improve their compliance and adherence to treatment. While our study focused on PAP users, we believe these results may be generalised more broadly in terms of the role online tools can have in improving medical treatment compliance overall.”
Adam Benjafield, PhD – ResMed Vice President Medical Affairs
Empowering the sleep apnoea patient.
PwC, 2016.
The study: Anonymous daily-usage data was analysed from over 23,000 patients during a 3-month period in Germany, the UK and Ireland on CPAP or automatic positive airway pressure (APAP) therapy for sleep apnoea.2 Patients were treated by sleep clinics and home care providers, and were all monitored via telemonitoring by their nurse or physician. Over 1,800 of these patients were also registered to ResMed’s myAir digital self-monitoring programme.
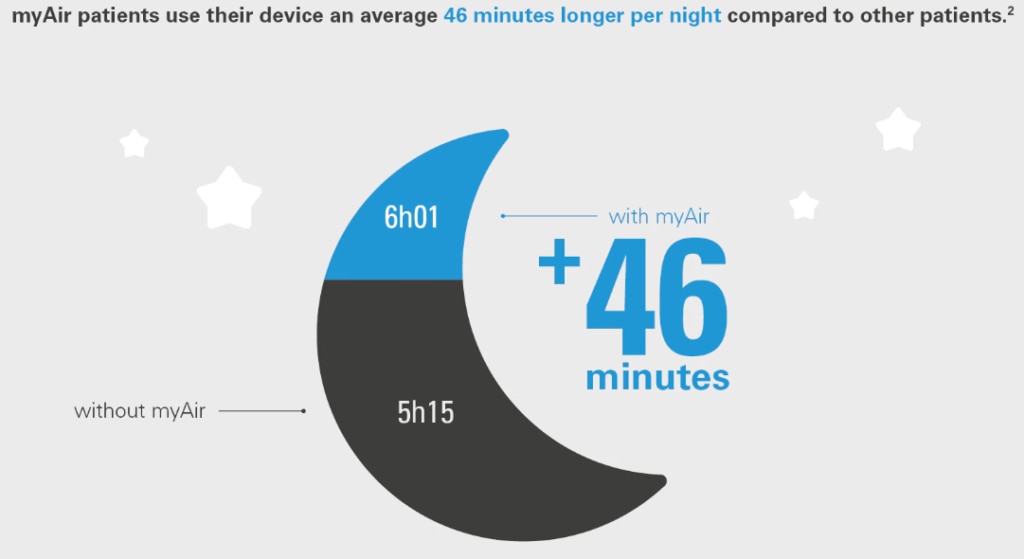
Findings: PwC’s research showed that patients who use online self-monitoring tools also use their devices longer per night.
- Patients who use myAir use their device on average 46 minutes more per night compared to other patients.2
- The average adherence to CPAP treatment for new patients in their first week of treatment is 76% for myAir patients compared to 71% for other patients.3
“In recent years, the introduction of telemonitoring has given sleep clinics and home care providers a tool to proactively intervene to help patients starting CPAP treatment. With myAir, telemonitoring has been taken to the next level, and this research has now confirmed that patients who use it show significantly and measurably better adherence and usage than other patients.”
Christian Käfling, PwC
A telehealth program for CPAP adherence reduces labour and yields similar adherence and efficacy when compared to standard care.
Munafo D, et al. Sleep Breath 2016.
The study: An evaluation of the effectiveness and coaching labour requirements of a web-based automated telehealth messaging programme compared to standard care in newly diagnosed OSA patients.
Findings: Telehealth programmes can reduce coaching needs while maintaining adherence.
The amount of coaching required per patient was significantly reduced from 58.3 minutes for the standard care group to 23.9 minutes for the telehealth group of patients. The majority of patients in this group stated the new approach met or exceeded their expectations.
Telemedicine-based proactive patient management during positive airway pressure therapy.
Holger Woehrle, et al. Somnologie, January 2017.
Results from ResMed Germany Healthcare, a German home care provider
The study: Data from a large German homecare provider was used to investigate the impact of a proactive patient management programme supported by remote access to PAP therapy data on therapy termination compared with standard care. The proactive strategy used data from AirView. Patients receiving their first PAP therapy were included and analysed in matched pairs, with 3,401 patients included in each group.
Findings: A telemedicine-based proactive management strategy compared with standard care of PAP patients was associated with a lower long-term therapy termination rate.
- In the first year of PAP therapy, the overall therapy termination rate was significantly lower (5.4% vs 11.0%; p < 0.001) and time to therapy termination was significantly longer (348 ∓ 58 vs 337 ∓ 76 days; p < 0.05) in the proactive versus standard care group.
- Cox proportional hazard analysis revealed a significantly reduced risk of PAP termination in the proactive versus the standard care group (hazard ratio 0.48, 95% confidence interval 0.4–0.57).
- Findings were consistent in subanalyses according to gender, type of device and insurance status, and in patients aged ≥40 years. However, in the subgroup of patients aged younger than 40 years, the risk of PAP termination was similar in the proactive and standard groups.
Retrospective descriptive study of CPAP adherence associated with use of the ResMed myAir application.
S Lynch, et al. ResMed Science Center, ResMed Ltd, Sydney, Australia, 2015.
The study: A ResMed retrospective descriptive study of myAir usage data collected from 2,343 de-identified patient records.
Findings: ResMed’s myAir digital self-monitoring programme was linked to greater CPAP adherence.
- Researchers found that 83.9% of new CPAP users who received standard care and used the ResMed myAir application achieved Medicare adherence in the first 90 days of their treatment.
- Equally impressive, 75.4% of users achieved adherence in 30 days, with a median time to achieve Medicare adherence of 23 days.
Additional Reading
- Wozniak DR, et al. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Publication, 2014.
- Konikkara J, et al. Early recognition of obstructive sleep apnea in patients hospitalized with COPD exacerbation is associated with reduced readmission. Hospital Practice, 2016.
- Kuna ST, et al. Web-Based Access to Positive Airway Pressure Usage with or without an Initial Financial Incentive Improves Treatment Use in Patients with Obstructive Sleep Apnea. Sleep, 2015.
Support for investigator initiated research
ResMed believes in the need to support ethical, independent clinical research, conducted by qualified third-party investigators.
More research in SDB

Narval CC *
There’s a growing body of clinical research that demonstrates the efficacy and compliance of mandibular repositioning devices (MRDs) in treating obstructive sleep apnoea and snoring

FACE study
The FACE study will provide long-term data on morbidity and mortality of heart failure (both HFrEF and HFpEF) patients using ASV**.

Big data analysis of CSA during CPAP therapy
Central sleep apnoea during CPAP therapy: first insights from a big data analysis.
*Please note the Narval CC mandibular advancement device is not available in England, Scotland or Wales.
This content is intended for health professionals only. Please refer to the instructions for use for relevant information related to any warnings and precautions to be considered before and during use of the products.
References:
**ASV therapy is contraindicated in patients with chronic, symptomatic heart failure (NYHA 2-4) with reduced left ventricular ejection fraction (LVEF ≤ 45%) and moderate to severe predominant central sleep apnoea.
- Crocker M et al. Patient Engagement Using New Technology to Improve Adherence to Positive Airway Pressure Therapy. Chest, 2016.
- Allen KY et al. The Clinician’s Guide to PAP Adherence. American Association for Respiratory Care, 2009.
- Price Waterhouse Coopers. Empowering the sleep apnoea patient: A study of how myAir users behave better. 2016.