Lumis™
Non-invasive ventilators
Non-invasive ventilator series for non-dependent patients (>13kg)1 with respiratory insufficiencies such as COPD. Lumis features individually-responsive technologies to deliver personalised ventilation. With wireless connectivity to AirViewTM, you can monitor and customise your patients’ settings remotely.




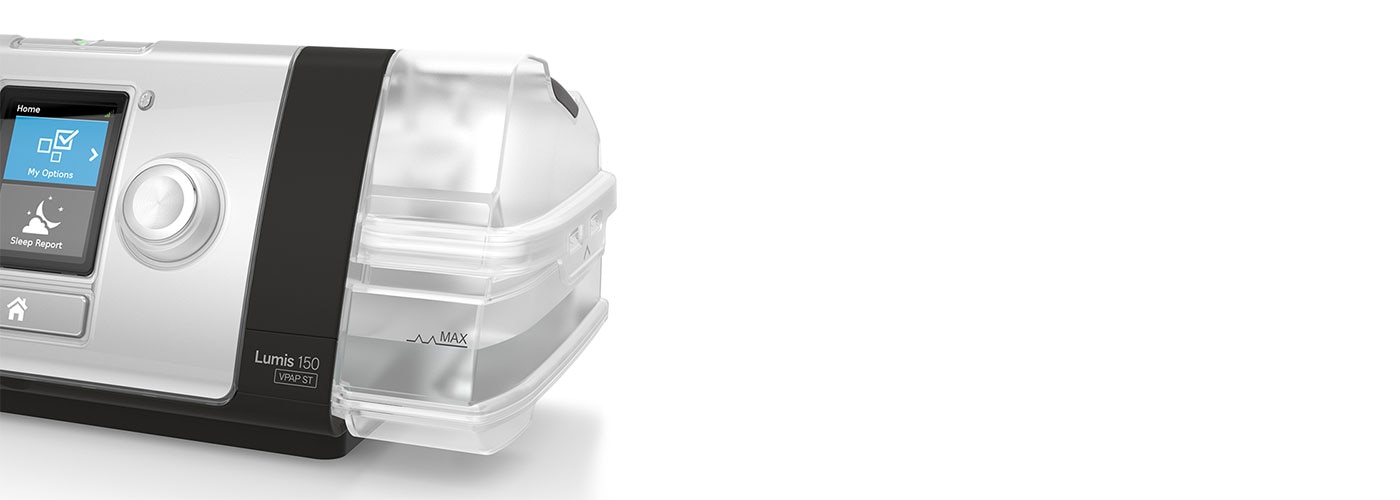
Personalisation simplified

With Lumis’ QuickNav feature you can easily toggle between the Settings and Monitoring screens, by simply double-clicking the home button on the device. Two Lumis models2 feature a set of fixed and adjustable alarms for reassurance.
Lumis displays your patient’s SpO2 and pulse rate3 on screen even before therapy has begun, so you can personalise the ventilator settings to suit their needs. Lumis’ individually responsive technologies allow you to fine-tune settings on a per patient basis.
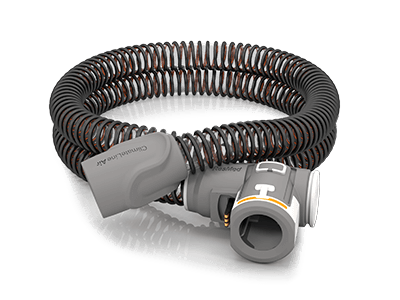
Automatic humidification
When used with a HumidAir™ heated humidifier and ClimateLineAir™ heated tube, Lumis delivers automatic humidification. Climate Control Auto mode comes pre-set with the temperature and humidity levels so you can set your patients up to receive the benefits of humidification.
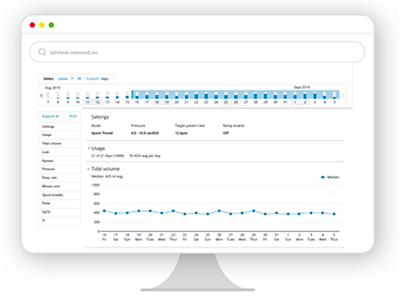
Connected care, better insight
Every Lumis device features built-in wireless connectivity so you can transfer therapy data directly to AirView, ResMed’s securely-hosted4, cloud-based patient management system for remote monitoring.
AirView’s Remote Assist feature gives you access to each patient’s device status and key settings (such as leak and humidification) to troubleshoot device-related issues quickly and easily.
Working together with Lumis
How to buy
Please contact our Customer Service department or your local representative for more information on obtaining ResMed products.
Warranty & services
Looking for service and warranty information on masks and accessories?
Find the answers to your questions in our resource centre.
Lumis 100 technical specifications
Lumis 100 S:
- CPAP
- S
Lumis 100 ST/ ST-A
- CPAP
- S
- T
- ST with optional iBR
- PAC
- Delivered pressure:
- Lumis 100 VPAP S & VPAP ST:
2–25 cm H2O (S, T, ST and PAC modes)
4–20 cm H2O (CPAP mode) - Lumis 100 VPAP ST-A:
2–30 cm H2O (S, T, ST and PAC modes)
4–20 cm H2O (CPAP mode)
- Lumis 100 VPAP S & VPAP ST:
- Respiratory rate: 5–50 bpm
- Supplemental oxygen: Recommended maximum flow: 15 L/min
- Settable alarms (Lumis 100 VPAP ST-A only)
- Vsync
- TiControl™
- Trigger and cycle
- Ramp
- Ramp Down
- Climate Control Auto
- Essentials mode
- SpO2 monitoring3
- Built-in wireless connectivity to AirView
- ResScan
- Weight:
- Lumis 100 VPAP S & VPAP ST
1106 g (device only)
1268 g (device with HumidAir humidifier) - Lumis 100 VPAP ST-A
1238 g (device only)
1336 g (device with HumidAir heated humidifier)
- Lumis 100 VPAP S & VPAP ST
- Dimensions (H x W x D):
116 mm x 205 mm x 150 mm (device only)
116 mm x 255 mm x 150 mm (device with HumidAir heated humidifier) - DC power supply: 24V/3.75A
- Sound pressure levels: 25 dBA with uncertainty of 2 dBA according to ISO 80601-2-70:2015 (CPAP mode)
- Aircraft use
Lumis 150 technical specifications
- CPAP
- S
- T
- ST with optional iBR
- PAC
- iVAPS1 (with iBR) and optional AutoEPAP
- Delivered pressure:
- Lumis 150 VPAP ST:
2–25 cm H2O (S, T, ST, PAC and iVAPS modes)
4–20 cm H2O (CPAP mode) - Lumis 150 VPAP ST-A:
2–30 cm H2O (S, T, ST, PAC, iVAPS modes)
4–20 cm H2O (CPAP mode)
- Lumis 150 VPAP ST:
- Respiratory rate: 5–50 bpm
- Supplemental oxygen: Recommended maximum flow 15 L/min – (CPAP, S, T, ST, PAC); 4 L/min (iVAPS)
- Settable alarms (Lumis 150 VPAP ST-A only)
- Vsync
- TiControl™
- Trigger and cycle
- Ramp
- Ramp Down
- Climate Control Auto
- Essentials mode
- SpO2 monitoring3
- Built-in wireless connectivity to AirView
- ResScan
- Weight:
- Lumis 150 VPAP ST:
1106 g (device only)
1268 g (device with HumidAir humidifier) - Lumis 150 VPAP ST-A:
1238 g (device only)
1336 g (device with HumidAir heated humidifier)
- Lumis 150 VPAP ST:
- Dimensions (H x W x D):
- 116 mm x 205 mm x 150 mm (device only)
116 mm x 255 mm x 150 mm (device with HumidAir heated humidifier)
- 116 mm x 205 mm x 150 mm (device only)
- DC power supply: 24V/3.75A
- Sound pressure levels: 25 dBA with uncertainty of 2 dB according to ISO 80601-2-70:2015 (CPAP mode)
- Aircraft use
Please refer to the user guide for relevant information related to any warnings and precautions to be considered before and during use of the product.
References:
- iVAPS therapy mode is indicated for patients weighing 30 kg and above. iVAPS is not available with Lumis 100
- Not available in all countries. Please contact your ResMed representative.
- Available when an SpO2 sensor is attached
- AirView was built to be secure and compliant with (EU) 2016/679 (General Data Protection Regulation) and national privacy laws. It uses data encryption technologies to secure patient data. ResMed obtained dual HDS/ISO 27001 certification for AirView to demonstrate our commitment to secure data processing and hosting and to ensure our teams and systems are operating at the highest standards, as verified by independent auditors.
- With Lumis, data is available one hour after the end of each therapy session.